Size of Baby at 13 Weeks in Utero
| Obstetric ultrasonography | |
|---|---|
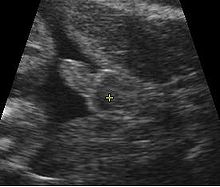
 Obstetric sonogram of a fetus at 16 weeks. The bright white circumvolve centre-correct is the caput, which faces to the left. Features include the forehead at 10 o'clock, the left ear toward the center at vii o'clock and the right hand covering the eyes at 9:00. | |
| Other names | prenatal ultrasound |
| ICD-9-CM | 88.78 |
| MeSH | D016216 |
| OPS-301 code | 3-032, 3-05d |
Obstetric ultrasonography, or prenatal ultrasound, is the use of medical ultrasonography in pregnancy, in which sound waves are used to create existent-time visual images of the developing embryo or fetus in the uterus (womb). The procedure is a standard function of prenatal care in many countries, equally it can provide a multifariousness of information about the health of the mother, the timing and progress of the pregnancy, and the health and evolution of the embryo or fetus.
The International Order of Ultrasound in Obstetrics and Gynecology (ISUOG) recommends that pregnant women have routine obstetric ultrasounds betwixt 18 weeks' and 22 weeks' gestational age (the anatomy browse) in order to ostend pregnancy dating, to measure the fetus so that growth abnormalities can be recognized quickly later in pregnancy, and to appraise for congenital malformations and multiple pregnancies (twins, etc).[1] Additionally, the ISUOG recommends that significant patients who desire genetic testing take obstetric ultrasounds between xi weeks' and thirteen weeks 6 days' gestational age in countries with resources to perform them (the nuchal scan). Performing an ultrasound at this early on stage of pregnancy tin can more accurately confirm the timing of the pregnancy, and tin likewise appraise for multiple fetuses and major congenital abnormalities at an before phase.[2] Research shows that routine obstetric ultrasound earlier 24 weeks' gestational age can significantly reduce the risk of declining to recognize multiple gestations and can improve pregnancy dating to reduce the adventure of labor induction for post-dates pregnancy. There is no difference, still, in perinatal expiry or poor outcomes for infants.[iii]
Terminology [edit]

Below are useful terms on ultrasound:[4]
- Echogenic — giving rise to reflections (echoes) of ultrasound waves
- Hyperechoic – more echogenic (brighter) than normal
- Hypoechoic – less echogenic (darker) than normal
- Isoechoic – the same echogenicity as some other tissue
- Transvaginal ultrasonography – Ultrasound is performed through the vagina
- Transabdominal ultrasonography – Ultrasound is performed across the abdominal wall or through the abdominal cavity
In normal state, each trunk tissue blazon, such as liver, spleen or kidney, has a unique echogenicity. Fortunately, gestational sac, yolk sac and embryo are surrounded by hyperechoic (brighter) body tissues.
Types [edit]
Traditional obstetric sonograms are done past placing a transducer on the abdomen of the meaning adult female. One variant, transvaginal sonography, is done with a probe placed in the woman'southward vagina. Transvaginal scans usually provide clearer pictures during early pregnancy and in obese women. Also used is Doppler sonography which detects the heartbeat of the fetus. Doppler sonography tin can be used to evaluate the pulsations in the fetal middle and bloods vessels for signs of abnormalities.[five]
3D ultrasound [edit]
Modern 3D ultrasound images provide greater detail for prenatal diagnosis than the older 2D ultrasound technology.[6] While 3D is popular with parents desiring a prenatal photograph as a keepsake,[vii] both 2nd and 3D are discouraged by the FDA for non-medical apply,[8] but there are no definitive studies linking ultrasound to any adverse medical effects.[9] The following 3D ultrasound images were taken at different stages of pregnancy:
-
3D Ultrasound of fetal movements at 12 weeks
-

Fetus at 17 weeks
-

Fetus at xx weeks
Medical uses [edit]
Early pregnancy [edit]
A gestational sac tin be reliably seen on transvaginal ultrasound by five weeks' gestational age (approximately 3 weeks after ovulation). The embryo should be seen by the time the gestational sac measures 25 mm, virtually v-and-a-half weeks.[10] The heartbeat is usually seen on transvaginal ultrasound past the fourth dimension the embryo measures 5 mm, merely may not exist visible until the embryo reaches 19 mm, around 7 weeks' gestational age.[5] [11] [12] Coincidentally, about miscarriages also happen past 7 weeks' gestation. The rate of miscarriage, especially threatened miscarriage, drops significantly after normal heartbeat is detected, and after xiii weeks.[13]
-
Embryo at 5 weeks and ane day of gestational age (at top left) with discernible heartbeat.
-

Embryo at five weeks and v days of gestational age with discernible heartbeat.
First trimester [edit]
In the first trimester, a standard ultrasound examination typically includes:[12]
- Gestational sac size, location, and number
- Identification of the embryo and/or yolk sac
- Measurement of fetal length (known as the crown-rump length)
- Fetal number, including number of amnionic sacs and chorionic sacs for multiple gestations
- Embryonic/fetal cardiac activity
- Cess of embryonic/fetal anatomy appropriate for the offset trimester
- Evaluation of the maternal uterus, tubes, ovaries, and surrounding structures
- Evaluation of the fetal nuchal fold, with consideration of fetal nuchal translucency assessment
2d and third trimester [edit]
In the second trimester, a standard ultrasound test typically includes:[12]
- Fetal number, including number of amnionic sacs and chorionic sacs for multiple gestations
- Fetal cardiac activity
- Fetal position relative to the uterus and cervix
- Location and appearance of the placenta, including site of umbilical cord insertion when possible
- Amnionic fluid volume
- Gestational age cess
- Fetal weight estimation
- Fetal anatomical survey
- Evaluation of the maternal uterus, tubes, ovaries, and surrounding structures when appropriate
Dating and growth monitoring [edit]

Biparietal diameter is taken as the maximal transverse diameter of in a visualization of the horizontal plane of the head.

Gestational historic period is usually adamant by the engagement of the adult female'south final menstrual menstruum, and bold ovulation occurred on day xiv of the menstrual bike. Sometimes a woman may exist uncertain of the date of her final menstrual period, or in that location may be reason to doubtable ovulation occurred significantly earlier or later than the fourteenth day of her cycle. Ultrasound scans offering an alternative method of estimating gestational historic period. The nearly accurate measurement for dating is the crown-rump length of the fetus, which tin can be done between 7 and 13 weeks of gestation. Afterward thirteen weeks of gestation, the fetal age may be estimated using the biparietal diameter (the transverse diameter of the caput, across the two parietal bones), the head circumference, the length of the femur, the crown-heel length (head to heel), and other fetal parameters.[ citation needed ] Dating is more accurate when done earlier in the pregnancy; if a later scan gives a dissimilar estimate of gestational age, the estimated age is not normally changed but rather it is causeless the fetus is not growing at the expected rate.[v]
The abdominal circumference of the fetus may also be measured. This gives an estimate of the weight and size of the fetus and is important when doing series ultrasounds to monitor fetal growth.[five]
Fetal sex discernment [edit]
Sonogram of male person fetus, with scrotum and penis in center of image
The sex of the fetus may exist discerned by ultrasound equally early as 11 weeks' gestation. The accuracy is relatively imprecise when attempted early on.[15] [16] [17] After 13 weeks' gestation, a high accurateness of between 99% and 100% is possible if the fetus does not display intersex external characteristics.[18]
The following is accuracy data from two hospitals:
| Gestational Age | King's College Hospital Medical School[16] | Taipei City Hospital & Li Shin Hospital[17] |
|---|---|---|
| eleven weeks | lxx.three% | 71.9% |
| 12 weeks | 98.7% | 92% |
| 13 weeks | 100% | 98.3% |
Influencing factors [edit]
The accurateness of fetal sex discernment depends on:[15]
- Gestational age
- Precision of sonographic machine
- Expertise of the operator
- Fetal posture
Ultrasonography of the cervix [edit]

Fetus at xiv weeks (profile)

Fetus at 14 weeks with avant-garde imaging filters
Obstetric sonography is useful in the cess of the cervix in women at risk for premature birth. A curt neck preterm is associated with a college gamble for premature delivery: At 24 weeks' gestation, a cervix length of less than 25 mm defines a risk group for spontaneous preterm nascence. Further, the shorter the neck, the greater the risk.[xix] Cervical measurement on ultrasound also has been helpful to utilize ultrasonography in patients with preterm contractions, as those whose cervical length exceeds 30 mm are unlikely to evangelize within the next week.[20]
Aberration screening [edit]
In near countries, routine pregnancy sonographic scans are performed to notice developmental defects before birth. This includes checking the condition of the limbs and vital organs, as well as (sometimes) specific tests for abnormalities. Some abnormalities detected past ultrasound can be addressed past medical treatment in utero or by perinatal care, though indications of other abnormalities tin lead to a conclusion regarding abortion.
Perhaps the most common such test uses a measurement of the nuchal translucency thickness ("NT-test", or "Nuchal Scan"). Although 91% of fetuses affected by Down's syndrome showroom this defect, 5% of fetuses flagged past the test do non accept Downwards syndrome.
Ultrasound may also detect fetal organ bibelot. Usually scans for this type of detection are done around xviii to 23 weeks of gestational age (called the "anatomy browse", "anomaly browse," or "level 2 ultrasound"). Some resources indicate that there are clear reasons for this and that such scans are likewise clearly benign because ultrasound enables clear clinical advantages for assessing the developing fetus in terms of morphology, bone shape, skeletal features, fetal centre function, volume evaluation, fetal lung maturity,[21] and general fetus well being.[22]
Second-trimester ultrasound screening for aneuploidies is based on looking for soft markers and some predefined structural abnormalities. Soft markers are variations from normal anatomy, which are more common in aneuploid fetuses compared to euploid ones. These markers are often non clinically significant and do not cause adverse pregnancy outcomes.[23]
Safety bug [edit]
3D rendering of the fetal spine in a scan at xix weeks of pregnancy
Electric current show indicates that diagnostic ultrasound is rubber for the unborn child, dissimilar radiographs, which use ionizing radiation. Randomized controlled trials have followed children up to ages viii–9, with no significant differences in vision, hearing, schoolhouse operation, dyslexia, or speech communication and neurologic development past exposure to ultrasound.[24] In i randomized trial, the children with greater exposure to ultrasound had a reduction in perinatal mortality, and was attributed to the increased detection of anomalies in the ultrasound group.[24]
The 1985 maximum power allowed by the U.S. Nutrient and Drug Administration (FDA) of 180 milliwatts per square cm[25] is well under the levels used in therapeutic ultrasound, but still higher than the thirty-fourscore milliwatts per foursquare cm range of the Statison Five veterinary LIPUS device.[26]
Doppler ultrasonography examinations has a thermal index (TI) of about 5 times that of regular (B-mode) ultrasound examinations.[24] Several randomized controlled trials have reported no association betwixt Doppler exposure and nascence weight, Apgar scores, and perinatal mortality. One randomized controlled trial, however, came to the effect of a higher perinatal decease rate of normally formed infants built-in after 24 weeks exposed to Doppler ultrasonography (RR 3.95, 95% CI 1.32–11.77), but this was not a primary outcome of the report, and has been speculated to be due to chance rather than a harmful effect of Doppler itself.[24]
The FDA discourages its use for non-medical purposes such as fetal keepsake videos and photos, even though it is the same technology used in hospitals.[27]
The American Institute of Ultrasound in Medicine recommends spectral Doppler only if M-mode sonography is unsuccessful, and even then simply briefly, due to the acoustic intensity delivered to the fetus.[28]
History [edit]
Polaroid photograph of an obstetric ultrasound taken in 1985.
Scottish doctor Ian Donald was one of the pioneers of medical use of ultrasound. His article "Investigation of Intestinal Masses past Pulsed Ultrasound" was published in The Lancet in 1958.[29] Donald was Regius Professor of Midwifery at the University of Glasgow.[30] [ cocky-published source? ]
In 1962, David Robinson, George Kossoff, George Radovanovich, and Dr William Garrett were the beginning in the world to identify a number of foetal anatomical structures from high frequency sound wave imaging.[31] [32]
In 1962, after about ii years of work, Joseph Holmes, William Wright, and Ralph Meyerdirk adult the starting time compound contact B-mode scanner. Their work had been supported by U.S. Public Health Services and the University of Colorado. Wright and Meyerdirk left the university to course Physionic Applied science Inc., which launched the first commercial hand-held articulated arm chemical compound contact B-mode scanner in 1963.[33] [ self-published source? ] This was the start of the near popular design in the history of ultrasound scanners.
Obstetric ultrasound has played a significant role in the evolution of diagnostic ultrasound technology in general. Much of the technological advances in diagnostic ultrasound technology are due to the drive to create better obstetric ultrasound equipment. Acuson Corporation's pioneering piece of work on the development of Coherent Paradigm Formation helped shape the evolution of diagnostic ultrasound equipment every bit a whole.[ commendation needed ]
In March and April 2015, a mail by a pregnant woman named Jen Martin (née Primal) and her married man to YouTube, which had been viewed at least 2 million times and had many likes, showed the fourteen-week-onetime fetus clapping repeatedly to the vocal, sung by the parents, "If You're Happy And You lot Know It." It was afterwards revealed that the video- while not a fake- had been somewhat edited to bear witness more fetal claps than likely occurred. It is not unprecedented for fetuses of that age to make momentary movements that could be repeated once or twice beyond the initial movement, according to experts, but to repeat such a movement more than that- especially purposefully- would not likely be viable at that point.[34] [35] [36]
Society and culture [edit]
The increasingly widespread utilise of ultrasound technology in monitoring pregnancy has had a swell impact on the way in which women and societies at large conceptualise and experience pregnancy and childbirth.[37] The pervasive spread of obstetric ultrasound engineering science effectually the world and the conflation of its use with creating a 'safe' pregnancy too every bit the ability to see and decide features similar the sex activity of the fetus affect the way in which pregnancy is experienced and conceptualised.[37] This "technocratic takeover"[37] of pregnancy is non limited to western or developed nations only also affects conceptualisations and experiences in developing nations and is an instance of the increasing medicalisation of pregnancy, a miracle that has social also as technological ramifications.[37] Ethnographic research concerned with the use of ultrasound technology in monitoring pregnancy can show us how it has changed the embodied experience of expecting mothers around the globe.[37]
Recent studies accept stressed the importance of framing "reproductive health matters cantankerous-culturally", particularly when agreement the "new phenomenon" of "the proliferation of ultrasound imaging" in developing countries.[38] In 2004, Tine Gammeltoft interviewed 400 women in Hanoi's Obstetrics and Gynecology Hospital; each "had an boilerplate of 6.vi scans during her pregnancy", much higher than five years prior when "a pregnant woman might or might not have had a single scan during her pregnancy" in Vietnam.[38] Gammeltoft explains that "many Asian countries" see "the foetus as an ambiguous being" unlike in Western medicine where it is common to think of the foetus equally "materially stable".[38] Therefore, although women, particularly in Asian countries, "express intense uncertainties regarding the safety and credibility of this technology", it is overused for its "immediate reassurance".[38]
Meet too [edit]
- 3D ultrasound
- Doppler fetal monitor
- Global Library of Women's Medicine
- Gynecologic ultrasonography
References [edit]
- ^ Salomon, LJ; Alfirevic, Z; Berghella, Five; Bilardo, C; Hernandez-Andrade, E; Johnsen, SL; Kalache, K; Leung, K.-Y.; Malinger, G; Munoz, H; Prefumo, F; Toi, A; Lee, W (2010). "Practise guidelines for performance of the routine mid-trimester fetal ultrasound scan". Ultrasound Obstet Gynecol. 37 (1): 116–126. doi:10.1002/uog.8831. PMID 20842655. S2CID 10676445.
- ^ Salomon, LJ; Alfirevic, Z; Bilardo, CM; Chalouhi, GE; Ghi, T; Kagan, KO; Lau, TK; Papageorghiou, AT; Raine-Fenning, NJ; Stirnemann, J; Suresh, S; Tabor, A; Timor-Tritsch, IE; Toi, A; Yeo, Chiliad (2013). "ISUOG Exercise Guidelines: performance of first-trimester fetal ultrasound scan". Ultrasound Obstet Gynecol. 41 (one): 102–113. doi:10.1002/uog.12342. PMID 23280739. S2CID 13593.
- ^ Whitworth, M; Bricker, 50; Mullan, C (2015). "Ultrasound for fetal cess in early on pregnancy". Cochrane Database of Systematic Reviews (7): CD007058. doi:x.1002/14651858.CD007058.pub3. PMC4084925. PMID 26171896.
- ^ Zwingenberger, Allison (10 April 2007). "What do hyperechoic and hypoechoic mean?". DVM Journals.
- ^ a b c d Woo, Joseph (2006). "Why and when is Ultrasound used in Pregnancy?". Obstetric Ultrasound: A Comprehensive Guide . Retrieved 2007-05-27 .
- ^ Dimitrova V, Markov D, Dimitrov R (2007). "[3D and 4D ultrasonography in obstetrics]". Akush Ginekol (Sofiia) (in Bulgarian). 46 (ii): 31–40. PMID 17469450.
- ^ Sheiner E, Hackmon R, Shoham-Vardi I, et al. (2007). "A comparison between acoustic output indices in 2D and 3D/4D ultrasound in obstetrics". Ultrasound Obstet Gynecol. 29 (iii): 326–8. doi:10.1002/uog.3933. PMID 17265534. S2CID 41853089.
- ^ Rados C (January–February 2004). "FDA Cautions Against Ultrasound 'Emblem' Images". FDA Consumer Magazine. Archived from the original on thirteen May 2009. Retrieved 28 Feb 2012.
- ^ Kempley R (9 August 2003). "The Grin Before They Carry It; Peek-a-Boo: Prenatal Portraits for the Ultrasound Set". Washington Post. Archived from the original on ii November 2012.
- ^ Doubilet, Peter M.; Benson, Carol B.; Bourne, Tom; Blaivas, Michael (2013-10-10). Campion, Edward W. (ed.). "Diagnostic Criteria for Nonviable Pregnancy Early in the Start Trimester". New England Journal of Medicine. 369 (fifteen): 1443–1451. doi:x.1056/NEJMra1302417. ISSN 0028-4793. PMID 24106937.
- ^ Boschert, Sherry (2001-06-fifteen). "Broken-hearted Patients Often Want Very Early on Ultrasound Exam". OB/GYN News. FindArticles.com. Retrieved 2007-05-27 .
- ^ a b c Cunningham, F; Leveno, KJ; Bloom, SL; Spong, CY; Dashe, JS; Hoffman, BL; Casey BM, BM; Sheffield, JS (2013). "Fetal Imaging". Williams Obstetrics, Twenty-Fourth Edition. McGraw-Loma.
- ^ "Miscarriage". A.D.A.Thou., Inc. 21 Nov 2010. Retrieved 28 Feb 2012.
- ^ Snijders, RJ.; Nicolaides, KH. (Jan 1994). "Fetal biometry at 14-40 weeks' gestation". Ultrasound Obstet Gynecol. 4 (1): 34–48. doi:10.1046/j.1469-0705.1994.04010034.x. PMID 12797224. S2CID 19399509.
- ^ a b Merz, Eberhard (2005). Ultrasound in obstetrics and gynecology (2nd ed.). Stuttgart: Thieme. p. 129. ISBN978-i-58890-147-7.
- ^ a b Efrat, Z.; Akinfenwa, O. O.; Nicolaides, K. H. (1999). "Offset-trimester conclusion of fetal gender by ultrasound". Ultrasound in Obstetrics and Gynecology. 13 (5): 305–7. doi:ten.1046/j.1469-0705.1999.13050305.x. PMID 10380292. S2CID 5364077.
- ^ a b Hsiao, C.H.; Wang, H.C.; Hsieh, C.F.; Hsu, J.J. (2008). "Fetal gender screening by ultrasound at 11 to 13+vi weeks". Acta Obstetricia et Gynecologica Scandinavica. 87 (1): 8–13. doi:x.1080/00016340701571905. PMID 17851807. S2CID 22374986.
- ^ Odeh, Marwan; Grinin, Vitali; Kais, Mohamad; Ophir, Ella; Bornstein, Jacob (2009). "Sonographic Fetal Sex Decision". Obstetrical & Gynecological Survey. 64 (1): l–57. doi:x.1097/OGX.0b013e318193299b. PMID 19099612. S2CID 205898633.
- ^ Iams, Jay D.; Goldenberg, Robert 50.; Meis, Paul J.; Mercer, Brian 1000.; Moawad, Atef; Das, Anita; Thom, Elizabeth; McNellis, Donald; et al. (1996). "The Length of the Neck and the Risk of spontaneous Premature Delivery". New England Journal of Medicine. 334 (ix): 567–72. doi:ten.1056/NEJM199602293340904. PMID 8569824.
- ^ Leitich, Harald; Brunbauer, Mathias; Kaider, Alexandra; Egarter, Christian; Husslein, Peter (1999). "Cervical length and dilatation of the internal cervical os detected by vaginal ultrasonography equally markers for preterm delivery: A systematic review". American Journal of Obstetrics and Gynecology. 181 (6): 1465–72. doi:x.1016/S0002-9378(99)70407-2. PMID 10601930.
- ^ Bhanu Prakash, Grand.N.; Ramakrishnan, A.One thousand.; Suresh, Due south.; Chow, T.Westward.P. (March 2002). "Fetal lung maturity analysis using ultrasound image features" (PDF). IEEE Transactions on It in Biomedicine. half-dozen (1): 38–45. doi:ten.1109/4233.992160. PMID 11936595. S2CID 14662967.
- ^ Layyous, Najeeb. "The Clinical Advantages of 3D and 4D Ultrasound - Dr Due north Layyous". www.layyous.com . Retrieved 21 March 2018.
- ^ Zare Mehrjardi, Mohammad; Keshavarz, Elham (2017-04-16). "Prefrontal Space Ratio—A Novel Ultrasound Marking in the Second Trimester Screening for Trisomy 21: Systematic Review and Meta-Analysis". Journal of Diagnostic Medical Sonography. 33 (4): 269–277. doi:10.1177/8756479317702619.
- ^ a b c d Houston, Laura E.; Odibo, Anthony O.; Macones, George A. (2009). "The safety of obstetrical ultrasound: a review". Prenatal Diagnosis. 29 (13): 1204–1212. doi:10.1002/pd.2392. ISSN 0197-3851. PMID 19899071. S2CID 26980283.
- ^ Freitas, Robert A. (1999). Nanomedicine. Austin, TX: Landes Bioscience. ISBN978-one-57059-645-ii. [ folio needed ]
- ^ "Statison V Operations Manual" (PDF). Statison Medical, Inc. 1997. Archived from the original (PDF) on 27 May 2008.
- ^ "Fetal Keepsake Videos". Nutrient and Drug Administration. Retrieved 2011-05-21 .
- ^ "Argument on Measurement of the Fetal Middle Rate". Audio Waves Weekly. American Institute of Ultrasound in Medicine. November 17, 2011.
When attempting to obtain fetal heart charge per unit with a diagnostic ultrasound system, the AIUM recommends using M-mode at outset because the fourth dimension-averaged acoustic intensity delivered to the fetus is lower with M-mode than with spectral Doppler. If this is unsuccessful, spectral Doppler ultrasound may exist used with the following guidelines: utilise spectral Doppler only briefly (eg, 4-5 center beats), and go along the thermal alphabetize (TIS for soft tissues in the first trimester and TIB for bones in second and third trimesters) as low equally possible, preferably below ane in accordance with the ALARA (as low as reasonably achievable) principle.
- ^ Donald, I; MacVicar, J; Brown, TG (1958). "Investigation of intestinal masses by pulsed ultrasound". Lancet. ane (7032): 1188–95. doi:10.1016/S0140-6736(58)91905-6. PMID 13550965.
- ^ Ian Donald'south paper in the Lancet in 1958 by Joseph Woo
- ^ "History of Sonography in Australia". Retrieved 17 August 2018.
- ^ "Bill Garrett: Obstetrics practitioner helped develop ultrasound". The Sydney Forenoon Herald. 10 December 2015. Retrieved 17 August 2018.
- ^ Woo, Joseph (2002). "A short History of the evolution of Ultrasound in Obstetrics and Gynecology". ob-ultrasound.net. Retrieved 2007-08-26 .
- ^ "Ultrasound Appears To Prove Fetus Clapping To 'If You're Happy And You lot Know Information technology'". Huffington Mail service. 30 March 2015.
- ^ "Ultrasound Shows Baby Clapping To 'If You're Happy And You Know It'". inquisitr.com. 28 March 2015. Retrieved 21 March 2018.
- ^ "Archived re-create". Archived from the original on 2015-04-13. Retrieved 2015-04-04 .
{{cite web}}: CS1 maint: archived copy as title (link) - ^ a b c d e [Gammeltoft, Tine, 2007, Sonography and Sociality – Obstetrical Ultrasound Imagining in Urban Vietnam, Medical Anthropology Quarterly, 21:ii, 133-153]
- ^ a b c d Gammeltoft, Tine (2007). "Sonography and Sociality: Obstetrical Ultrasound Imaging in Urban Vietnam". Medical Anthropology Quarterly. 21 (2): 133–53. doi:10.1525/maq.2007.21.ii.133. PMID 17601081.
External links [edit]
- RadiologyInfo: Obstetric Ultrasound Imaging
- AIUM statement on prudent use of Ultrasound
- The Global Library of Women's Medicine Imaging in Obstetrics and Gynecology link
Source: https://en.wikipedia.org/wiki/Obstetric_ultrasonography
0 Response to "Size of Baby at 13 Weeks in Utero"
Post a Comment